Does antidepressant overuse hinder our ability to heal PTSD?
- The pharmacological revolution promised us the ability to tame trauma with a pill.
- Some experts argue that the antidepressant paradigm ignores crucial realities about healing.
- Psychiatrist Bessel van der Kolk shares four non-pharmacological treatments that he believes deserve more attention.
Despite humankind’s intimate familiarity with tragedy and disaster, the concept of trauma has long confounded us. Throughout history, we’ve often attributed trauma’s toll to either a character flaw (the “cowardice” of shell-shocked soldiers) or a hereditary weakness (the many hysteria hypotheses of history). It wasn’t until the second half of the 20th century that we finally recognized this emotional and physical anguish isn’t the fault of the victim.
In fact, posttraumatic stress disorder (PTSD) didn’t find its way into the Diagnostic and Statistical Manual of Mental Disorders (DSM) until the manual’s third edition, which was published in 1980.
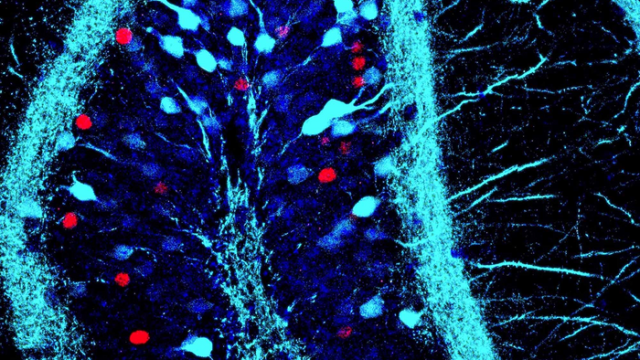
“We have learned that trauma is not just an event that took place sometime in the past; it is also the imprint left by that experience on mind, brain, and body. This imprint has ongoing consequences for how the human organism manages to survive in the present,” psychiatrist and neuroscientist Bessel van der Kolk writes in his book The Body Keeps Score.
This recognition came around the same time health researchers were discovering the role medication might play in mental health. The monoamine hypothesis — which proposes that a hormonal deficiency causes depression — was proposed in the early 1950s. The first report on a selective serotonin reuptake inhibitor (SSRI) — a popular type of antidepressant — debuted in the mid-1970s.
The pharmacotherapy revolution had arrived. It’s implicit promise: Even if we could not prevent tragedies or disasters, we could at least tame the specter of trauma with a daily pill ( so much quicker and easier than the drawn-out process of psychotherapy).
In the intervening decades, however, many experts have begun to wonder if our overenthusiasm for antidepressants has hindered the healing process for many survivors. They’re encouraging professionals to explore alternative, and perhaps more fruitful, methods of treatment.
Antidepressants and the placebo effect
For van der Kolk, who came of professional age after the Vietnam War, the pharmacological paradigm rests on two fundamental flaws. First, it ignores the human capacity to heal, regulate our own physiology, and establish protective factors through social conditioning (such as universal healthcare).
Second, it props up antidepressants as more effective than they are. As detailed in his book, van der Kolk once led a study that separated 88 PTSD patients into three groups. One group was given Prozac, another a placebo, and the final group underwent eye movement desensitization and reprocessing (EMDR) therapy. We’ll discuss the EMDR group in a moment, but for now, know that the Prozac group only showed a slight improvement over the placebo group.
Now, it’s worth clarifying this conclusion to prevent misreading; van der Kolk isn’t saying antidepressants are effectively overpriced sugar pills. In many PTSD studies, placebos demonstrate a remarkably high response rate. The reason for this isn’t necessarily that antidepressants are ineffective. It could be that the act of admitting one’s trauma and seeking help alone has tangible benefits.
But given that, even proponents of pharmacotherapy would likely agree with van der Kolk that our overenthusiasm for antidepressants may have stymied research into other equally effective treatments.
“After conducting numerous studies of medications for PTSD, I have come to realize that psychiatric medications have a serious downside, as they may deflect attention from dealing with the underlying issues,” van der Kolk writes.

4 promising interventions
In an interview with Big Think, van der Kolk shared some therapeutic approaches that he believes deserve either greater public attention or more exploration from researchers:
Psychotherapy. In psychotherapy (or talk therapy), patients develop a trusting relationship with their therapist and then work together to explore and solve underlying issues. There are many different techniques, but the gold standard today is cognitive behavioral therapy and its many iterations.
And unlike the other interventions on this list, psychotherapy has a substantial evidence base to suggest that it outperforms pharmacotherapeutic-only approaches.
For example, a 2019 meta-analysis published in JAMA Psychiatry combined data from 12 randomized clinical trials and more than 900 participants. It found that psychotherapy and pharmacotherapy were equally effective at the time of treatment. However, the benefits of psychotherapy lasted much longer. A combination of the two was also found to be effective.
“What’s very clear is that very good psychotherapy is actually quite helpful. Not to fix people, but helping people to acknowledge, ‘Oh my God, that was terrible what happened to me. And I need to take care of the wounds that I’m carrying inside myself,’” van der Kolk said.
He added, “This issue of self-compassion and really knowing that your reactions are understandable is a terribly important part of beginning to recover from trauma.”

EMDR. During EMDR treatment, a patient focuses on a traumatic memory while identifying the negative emotions and beliefs surrounding it. They then process the memory while engaging in side-to-side eye movement — usually by following the therapist’s pen or fingertip — until it is no longer troubling. Positive emotions and beliefs are then instilled while engaging in the same eye movement.
“Wiggling your fingers in front of peoples’ eyes as they think about the trauma made the trauma go away. This crazy eye movement desensitization actually changes the circuitry of the brain to interpret your current reality from a different angle. This had amazing effects on people being able to let go of what happened,” van der Kolk said.
Because EMDR is relatively new, its evidence base isn’t nearly as robust as psychotherapy’s. Still, early research has seen some positive results. In van der Kolk’s study, EMDR patients showed the lowest drops in PTSD scores, and they continued to improve months after the treatment. Other studies have found it as effective as other treatments (though not more so).
However, some experts recommend caution against widespread adoption, citing a lack of quality studies. Because of this, the American Psychological Association has given EMDR a conditional recommendation pending further research.
Yoga. PTSD can inhibit people’s lives by disconnecting their minds and bodies. Exercises like yoga and mindfulness, which focus on both, have been shown to help reestablish that link.
According to van der Kolk, “[o]ne of the clearest lessons from contemporary neuroscience is that our sense of ourselves is anchored in a vital connection with our bodies. We do not truly know ourselves unless we can feel and interpret our physical sensations; we need to register and act on these sensations to navigate safely through life.”
A 2018 meta-analysis published in Clinical Psychology Review combined 19 randomized control trials totaling more than 1,100 participants. Looking at yoga and mindfulness’s PTSD outcomes, it found a small, yet statistically significant, effect size in adult patients. They recommended both as a “promising complementary” to other treatments.

Psychotherapist Sabina Pillai demonstrates what a patient would experience in a therapy room at Field Trip, a psychedelic therapy clinic in as medical director Dr. Michael Verbora waits by her side in Toronto, Ontario, Canada, on August 28, 2020.
Psychedelics. Like EMDR, psychedelics don’t have a large base of evidence. As a Schedule 1 drug, getting permission to study them is a nightmare of paperwork and bureaucratic sludge.
Even so, intrepid researchers have managed to pull together small studies, and the preliminary results are hopeful if not conclusive. A study published in Nature Medicine explored MDMA-assisted psychotherapy with 79 participants. Two months after the study, 67% of the MDMA group no longer meet the criteria for PTSD (compared to 32% of the control group).
As van der Kolk explained: “MDMA allows people to see themselves with compassion. All these measures we have about self-perception and self-awareness just shoot up. And rather than blaming themselves, they’re able to say, ‘Yes, this is what happened to me, but it’s over.’” These results have caught the eye of larger organizations, such as John Hopkins University and the Department of Veteran Affairs, who are beginning their own trials into psychedelics.
We have learned that trauma is not just an event that took place sometime in the past; it is also the imprint left by that experience on mind, brain, and body.
– Bessel van der Kolk
No fixed path for healing PTSD
What are we to take from all of this? Is it that we’ve been duped by big pharma for decades, spending thousands on pills when all we needed was someone to talk to and yoga hosiery?
Not at all. Speaking broadly — because there are a lot of medications out there — SSRIs fare better than placebos in meta-analyses and systematic reviews. The effect sizes may be small to medium, but they are present in the data. And because some relief is better than no relief, organizations like the American Psychological Association and the National Institute of Health do recommend antidepressants conditionally, usually in combination with psychotherapy.
Rather, the takeaway is that antidepressants don’t work the same for every patient. The same is true for psychotherapy or any other treatment. But the more tools we understand and make available, the more individualized treatments psychiatrists can craft for their patients. Experts like van der Kolk simply want to take this approach even further — even recommending further research into approaches like neurofeedback therapy and drama therapy.
“But what’s important here is that one size doesn’t fit all. Different people need very different things. What worked for my last patient very well may not work for you,” van der Kolk said. “Everything is an experiment in life. And healing from trauma is an experiment.”
Learn more on Big Think+
With a diverse library of lessons from the world’s biggest thinkers, Big Think+ helps businesses get smarter, faster. To access Bessel van der Kolk’s full class for your organization, request a demo.