The prevalence of mental illness around the world
Mental illnesses are diagnosed by health professionals using manuals, which describe their symptoms, their context, and how they differ from similar conditions.
How are these manuals used? How are major mental illnesses described and diagnosed?
This article summarizes the major mental illnesses in the ICD-11 manual, the official worldwide classification.
Each section includes a summary of how the condition is medically diagnosed, a description of the symptoms, and other conditions that must be ruled out before making a diagnosis.
If you want to read the full criteria for diagnosing mental illnesses according to the ICD-11, you can find them here.
What are the different manuals in use?
Diagnosing a mental illness begins when people see a doctor or psychiatrist.
It can be difficult to define mental illnesses because they are conditions of the mind: they are diagnosed according to people’s symptoms and behavior. This means they can be subjective – they are dependent partly on people’s comfort seeing a doctor or psychiatrist, the training and experiences of healthcare professionals, and other cultural factors.
Two manuals are commonly used by doctors and psychiatrists to diagnose mental illnesses: the International Classification of Diseases (ICD) and the Diagnostic and Statistical Manual of Mental Disorders (DSM).
There are differences in how they are used.
The ICD is the official worldwide classification for healthcare and data collection. It is used by a wide range of healthcare professionals.
In contrast, the DSM was developed for psychiatrists in the United States, although its usage has expanded worldwide. It is intended to provide standardized guidelines for different psychiatrists who may have different judgments otherwise.1
Each of these manuals has been revised several times: the ICD is currently on its eleventh edition (known as ICD-11) as of 2019, while the DSM is currently on its fifth edition (DSM-5) as of 2013.
Both manuals provide criteria healthcare professionals can use to decide whether people have a particular mental illness.
These criteria include a description of the symptoms, their severity, and duration. They also explain how to decide between different illnesses with similar symptoms.
Both manuals mostly group mental illnesses similarly. For common mental illnesses, their criteria are usually identical or have minor differences, but in some cases, there are major differences.2
How common are mental illnesses?
In the chart, you can see the estimated prevalence of people who meet the criteria to be diagnosed with each category of mental illness.
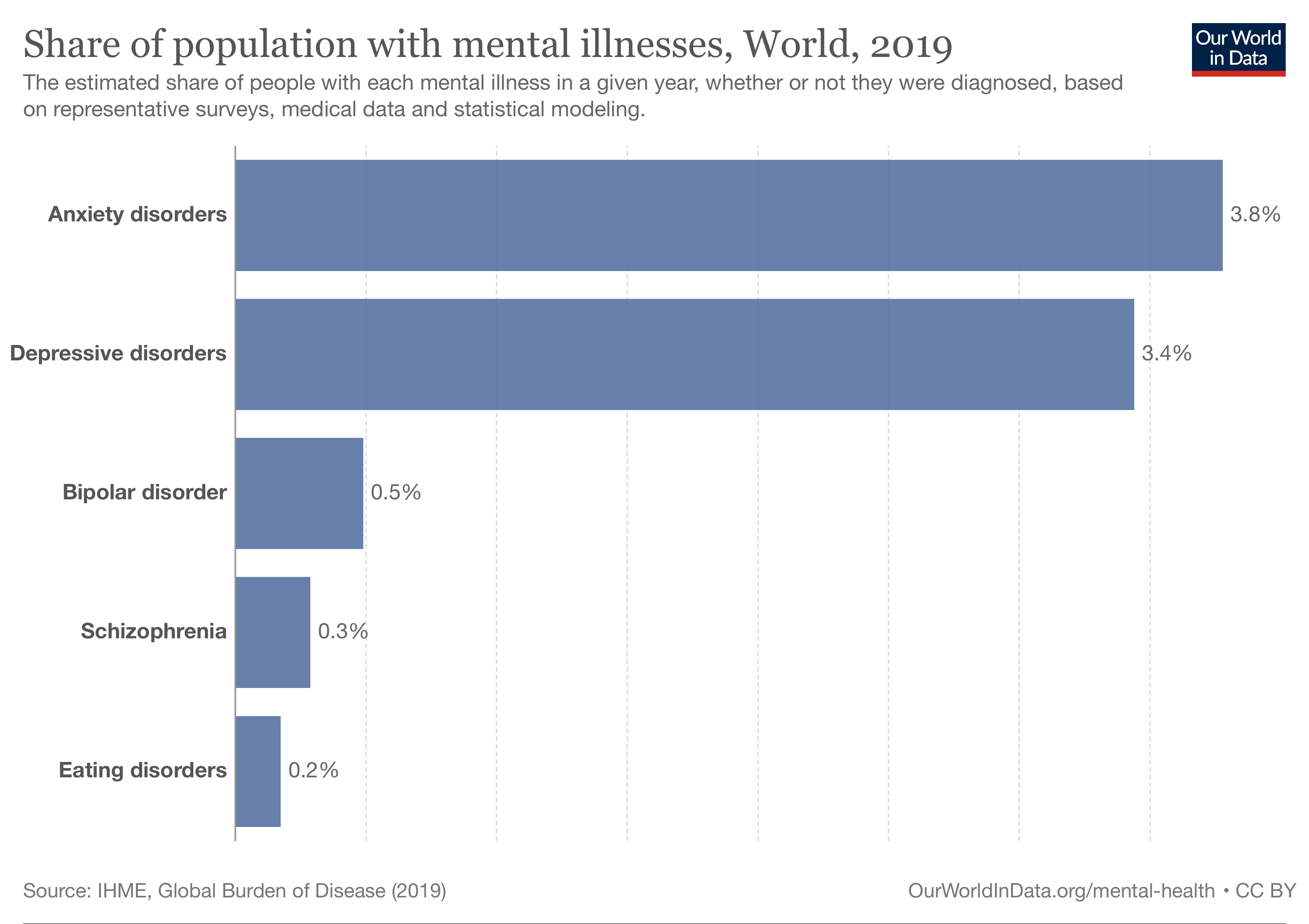
As you can see, anxiety disorders and depressive disorders are more common. It’s estimated that around 3–4% of people worldwide have had them in the past year.
Bipolar disorder, schizophrenia and eating disorders are less common. For example, it’s estimated that 0.3% of people have schizophrenia worldwide.
Schizophrenia and other primary psychotic disorders
Schizophrenia
Schizophrenia is a condition that involves significant problems in perceiving reality, difficulty with memory and attention, and changes in behavior and movement.3
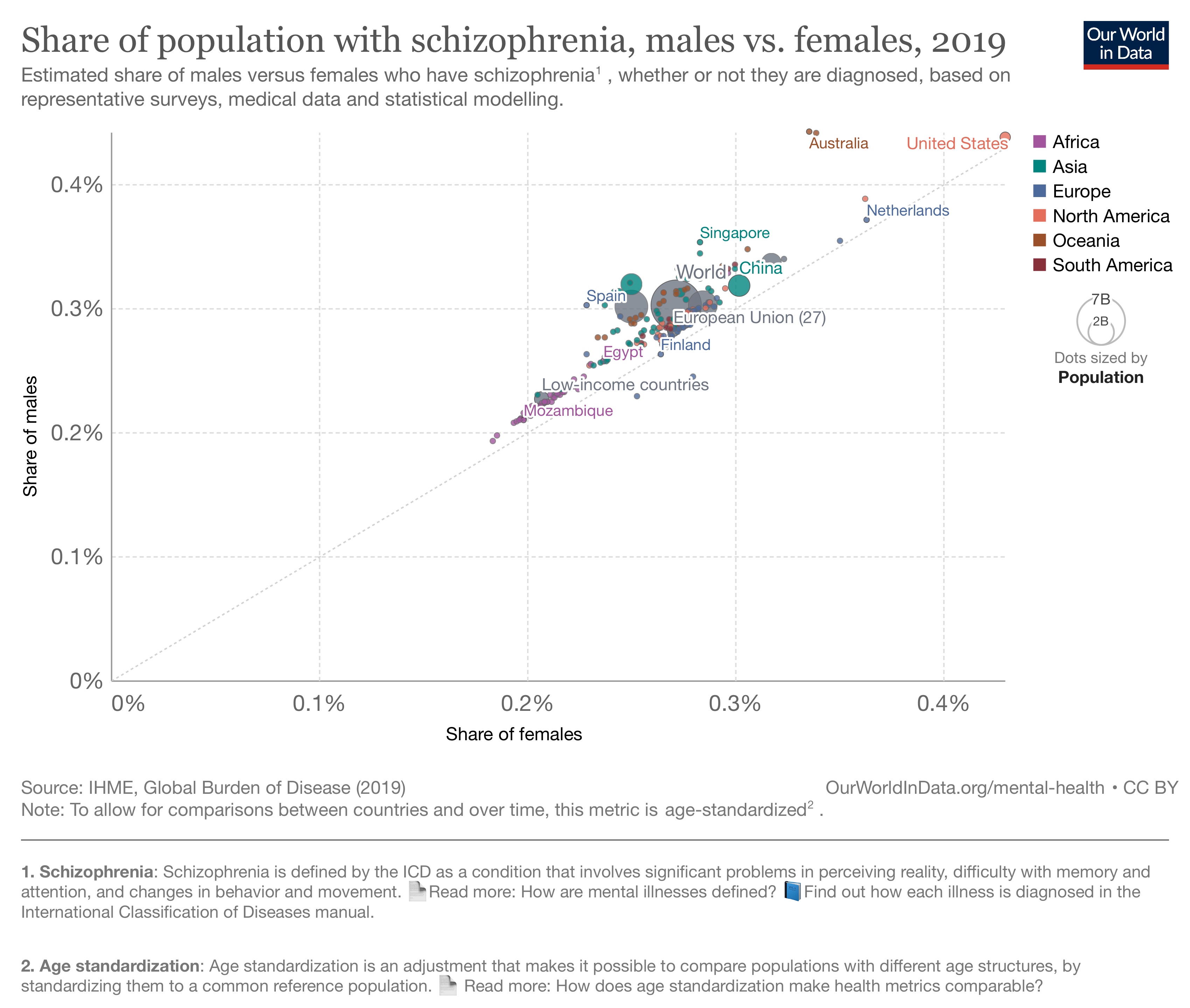
In the chart, you can see the rate of schizophrenia between genders. As the chart shows, around 0.2 to 0.5% of people are estimated to have schizophrenia across countries. Schizophrenia is relatively balanced between men and women, although in many countries it’s estimated to be slightly more common among men than women.
To diagnose schizophrenia, the patient must have at least two of the following symptoms for most of the time, lasting at least a month. They must have at least one symptom from a–d.
- persistent delusions
- persistent hallucinations
- disorganized thoughts that may result in incoherent speech
- experiences of control or passivity
- negative symptoms (such as flattening of emotions, loss of interest or motivation, lack of speech)
- disorganized behavior (i.e., behavior that is purposeless, or inappropriate emotional responses)
- changes in behavior and movement such as catatonic restlessness, posturing, wavy flexibility, negativism, mutism, stupor
The symptoms shouldn’t be caused by another medical condition or the use of substances or medication.
Mood disorders
The ICD manual describes two types of mood disorders: depressive disorders, and bipolar or related disorders.
Depressive disorders
Depressive disorders involve significant sadness or a loss of interest, along with several other symptoms.
But there are several types of depressive disorders, classified by the ICD manual. They are based on the specific symptoms, their severity, and duration.4
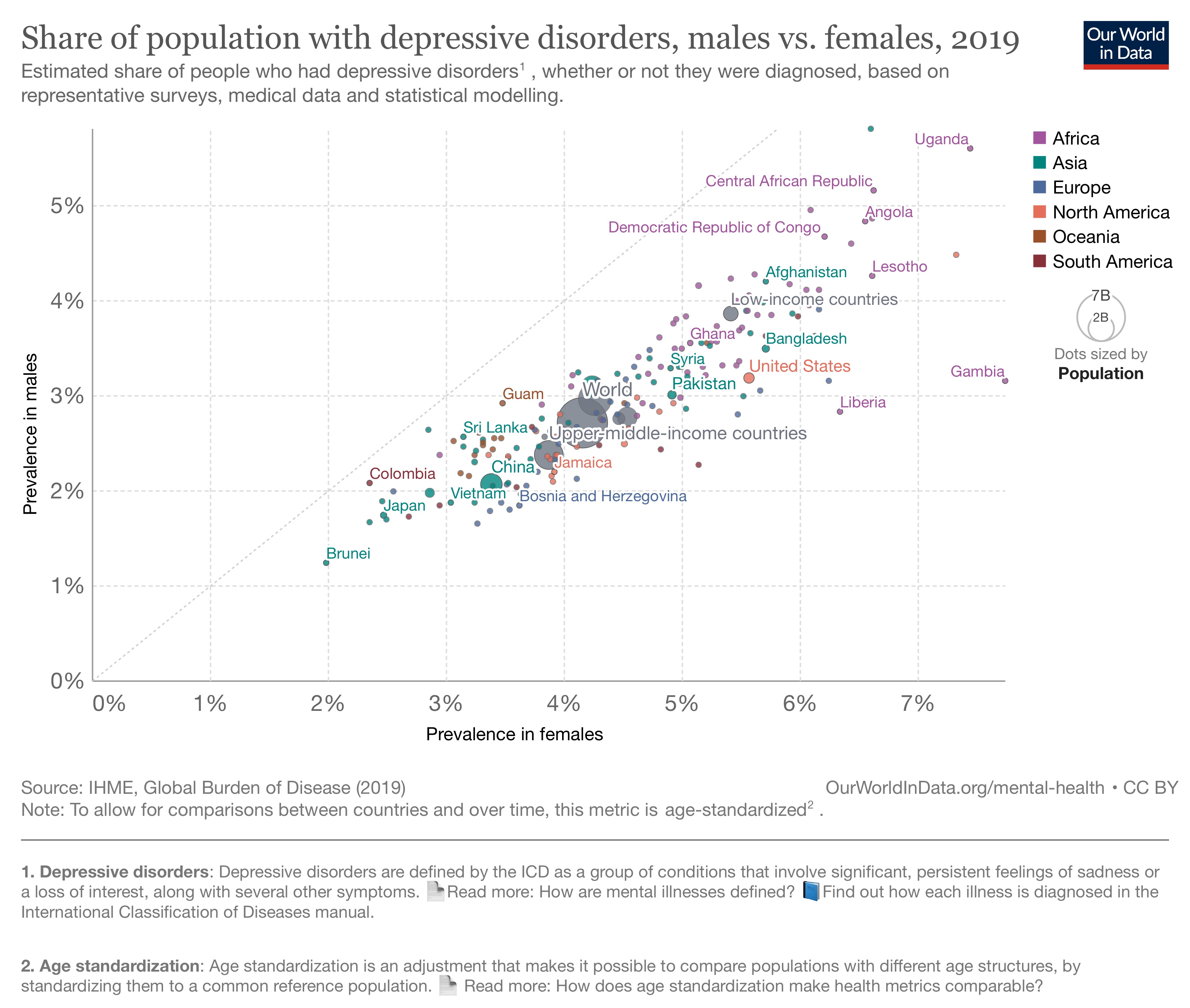
In the chart, you can see the prevalence of depressive disorders in men and women. As the chart shows, it’s estimated that depressive disorders were somewhat more common in women than men in all countries. Around 2–8% of women and 1–6% of men were estimated to have depressive disorders in the past year, across countries.
Major depression
Several types of depressive disorders involve having a major depressive episode, which can be mild, moderate, or severe.
To diagnose a major depressive episode, the patient must have had at least five of the symptoms listed below for most of the day, lasting nearly every day for at least 2 weeks.
At least one of them must be from a–b. The symptoms must also significantly affect their personal life, family, social, education, work, or other areas of their life – or only have a limited effect because of significant effort.
- Depressed mood (feeling down or sad). In children and adolescents, this may appear as irritability instead.
- Less interest or pleasure in activities that the person usually finds enjoyable
- Reduced ability to concentrate or make decisions
- Excessive feelings of low self-worth or inappropriate guilt that may be delusional
- Feeling hopelessness about the future
- Recurrent thoughts of death, thoughts about suicide, or evidence of attempted suicide
- Significant disruptions in sleeping
- Significant changes in appetite
- Changes in behavior and movement (being agitated or slowed down), which can be observed by others
- Reduced energy, fatigue or feeling tired after a minimum amount of effort
The symptoms shouldn’t be better accounted for by bereavement (the death of someone close), another medical condition, or the use of substances or medication.
Dysthymic disorder
Unlike major depression, dysthymic disorder involves having milder symptoms for a longer minimum period.
To diagnose a dysthymic disorder, the patient must have had a persistent depressed mood lasting at least two years, for most of the day, for the majority of days. In children and adolescents, this may appear as irritability instead. The symptoms must also significantly affect their personal life, family, social, education, work, or other areas – or only be limited because of significant effort.
In addition, they typically have additional symptoms such as:
- Less interest or pleasure in activities that the person usually finds enjoyable
- Reduced ability to concentrate or make decisions
- Excessive feelings of low self-worth, or inappropriate guilt that may be delusional
- Feeling hopelessness about the future
- Significant disruptions in sleeping
- Significant changes in appetite
- Reduced energy or fatigue
To be diagnosed, there should not have been a two-week period when they had enough symptoms to meet the criteria for a depressive episode, during the first two years of their symptoms. There should also not be any period without symptoms lasting two months or more.
They should not have a history of manic episodes, mixed episodes, or hypomanic episodes (which would meet the criteria of bipolar or related disorders; see the next section). The symptoms shouldn’t be caused by another medical condition or the use of substances or medications.
Bipolar and related disorders
Bipolar disorder involves two different sets of symptoms. One set is depressive symptoms, while the other involves significantly increased excitement, irritability, and energy. This second set of symptoms is classified as “manic episodes”, “mixed episodes”, or “hypomanic episodes or symptoms”.5
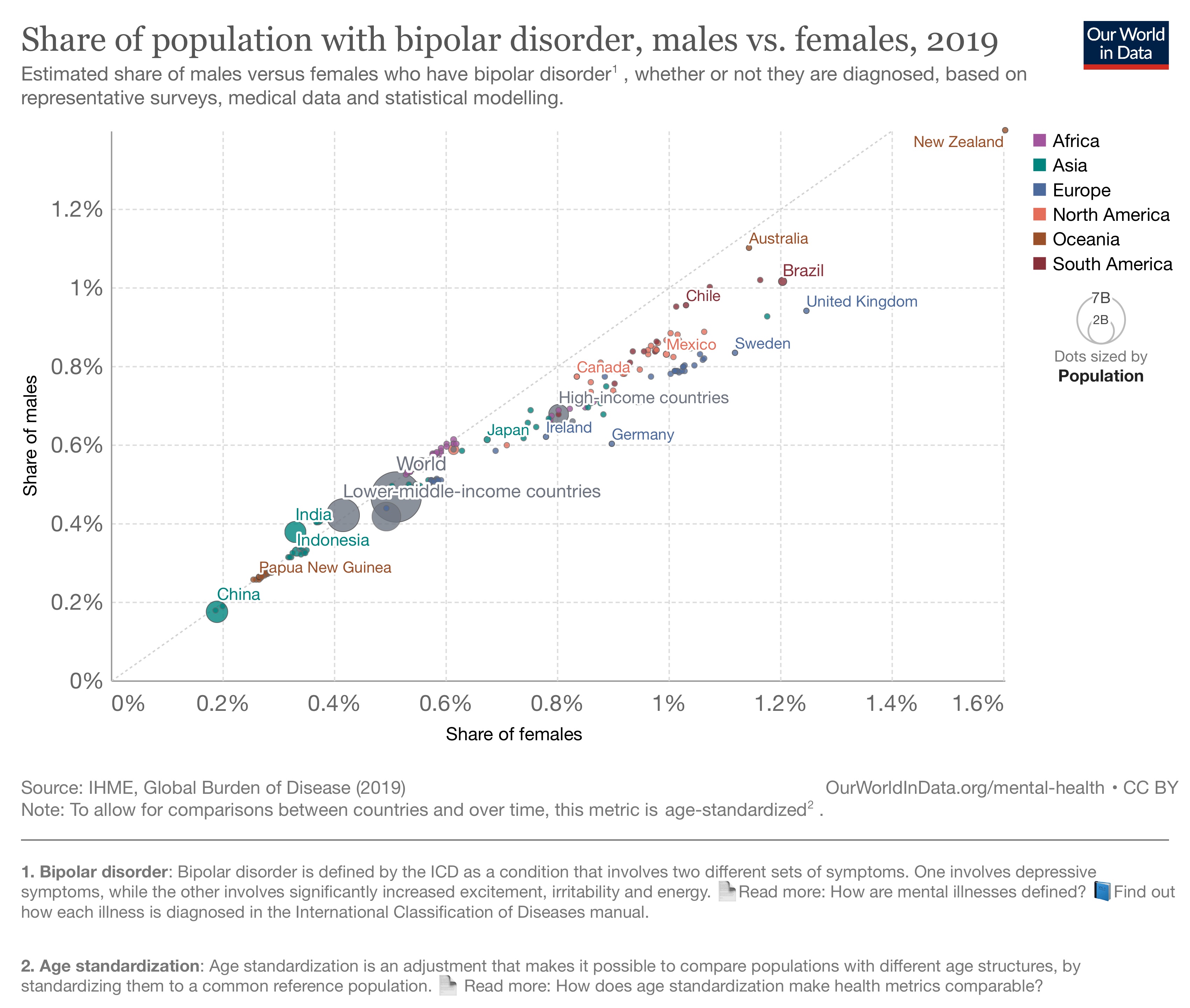
In the chart, you can see the prevalence of bipolar disorder in different countries. Overall, around 0.2–1.8% of people are estimated to have bipolar disorder. Bipolar disorder is relatively balanced between men and women, although in many countries it’s estimated to be slightly more common among women than men.
To diagnose someone with a manic episode, the patient must have the following symptoms for most of the day, nearly every day, for at least a week6.
- An extreme mood of euphoria, irritability, or a feeling of ‘expansiveness’.7
- Significantly increased activity or energy compared to their usual behavior.
Along with these, their behavior must include several of the following unusual symptoms.
- Increased talkativeness
- Racing thoughts or ideas, which may be illogical
- Increased self-esteem or grandiosity
- Less need for sleep
- Being easily distracted
- Impulsive, reckless behavior
- Increased sexual drive, sociability, or activity directed towards a goal
Their symptoms should not be due to another medical condition or the use of a substance or medication, and they shouldn’t fill the requirements for a mixed episode.
To be diagnosed, their symptoms must also significantly affect their personal life, family, social, education, work, or other areas of their life; or require intensive treatment to prevent them from harming themselves or others; or are accompanied by delusions or hallucinations.
Anxiety or fear-related disorders
There are many illnesses related to anxiety and fear. They are classified by the ICD manual as generalized anxiety disorder, panic disorder, agoraphobia, specific phobias, social anxiety disorder, separation anxiety disorder, selective mutism, and others.
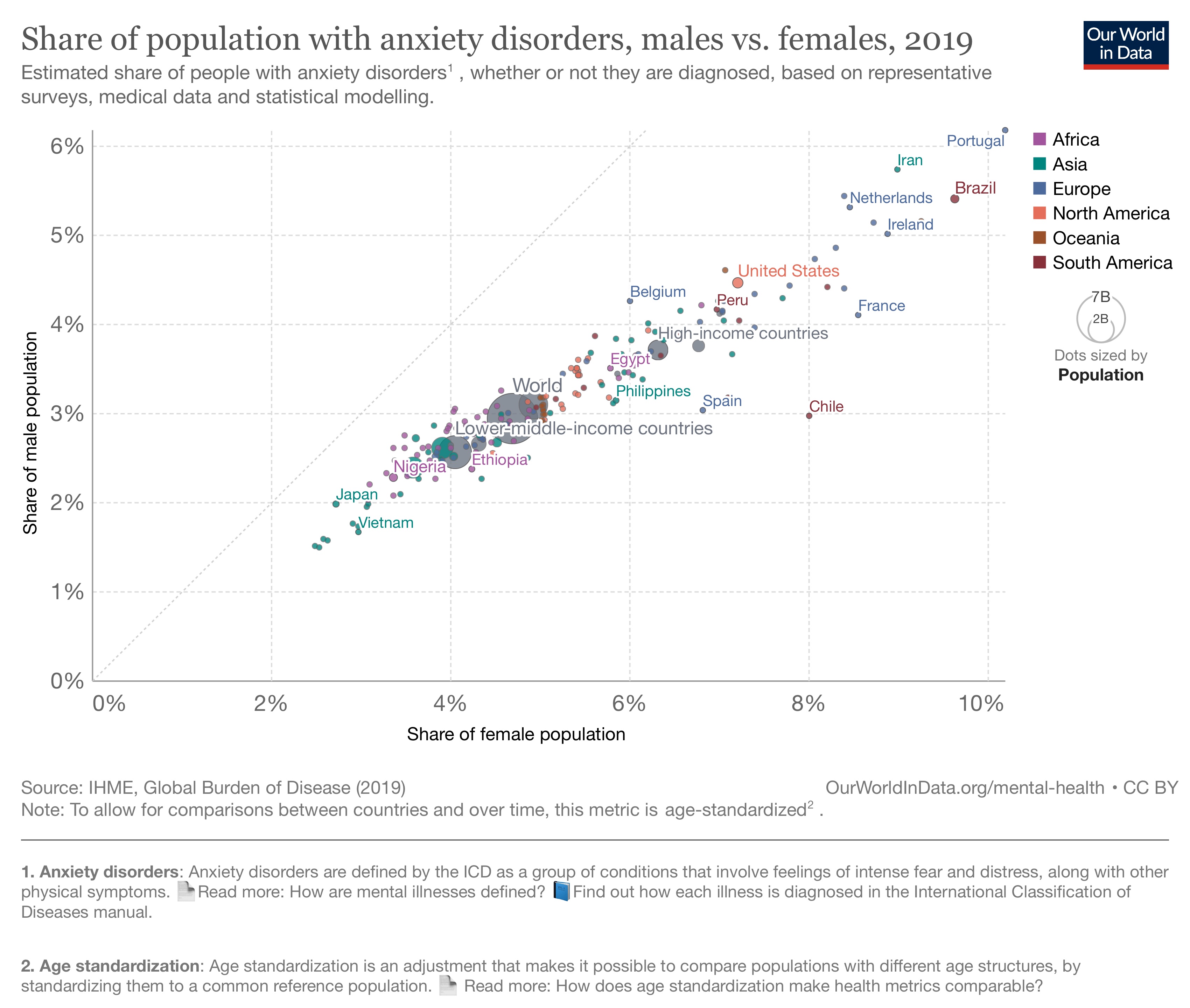
In the chart, you can see the estimated share of people who would meet the criteria for anxiety disorders in men and women. You can see that anxiety disorders are estimated to be more common in women than men in all countries. Around 2–11% of women and 2–7% of men were estimated to have anxiety disorders in the past year, across countries.
Generalized anxiety disorder
Generalized anxiety disorder involves persistent anxiety symptoms. The symptoms must also significantly affect their personal life, family, social, education, work, or other areas – or only be limited because of significant effort.
To be diagnosed with generalized anxiety disorder, patients must have either:
- Excessive worry about several aspects of everyday life, including work, finances, health, or family
- General anxiety that is not about particular events
Along with this, they must have additional symptoms such as:
- Muscle tension or physical restlessness
- Overactive physical symptoms such as nausea or abdominal distress, rapid heartbeat, sweating, trembling, shaking or dry mouth
- Feeling nervous, restless or being ‘on edge’
- Difficulty concentrating
- Being irritable
- Disruptions in sleeping
To be diagnosed, their symptoms must persist for at least several months, for the majority of days. They should not be better accounted for by another mental disorder, and should not be the result of another medical condition or the use of substances or medication.
Obsessive-compulsive and related disorders
This is a group of illnesses that involve symptoms of repetitive thoughts and behaviors, such as obsessions, intrusive thoughts, and preoccupations.
According to the ICD manual, the group includes: obsessive-compulsive disorder (OCD), body dysmorphic disorder, olfactory reference disorder, hypochondriasis, hoarding disorder, body-focused repetitive behavior disorder, and others.
Obsessive-compulsive disorder (OCD)
To be diagnosed with obsessive-compulsive disorder, the ICD manual explains that the patient must have repetitive and persistent obsessions and/or compulsions. These can be thoughts, images, or impulses/urges that feel intrusive and unwanted and are commonly linked to anxiety. The patient usually tries to ignore them, suppress them, or comply with them by performing repetitive behaviors or rituals.
To be diagnosed, these obsessions and compulsions must be time-consuming or significantly affect their personal life, family, social, education, work, or other areas – or are only limited because of significant effort.
Their symptoms should not be better accounted for by another mental disorder and should not be the result of another medical condition or the use of substances or medication.
Eating and feeding disorders
According to the ICD manual, eating disorders involve abnormal behaviors and preoccupations with food, along with strong concerns about body weight and shape.
In contrast, feeding disorders involve abnormal behaviors such as eating non-edible substances or regurgitating food without concerns about body weight or shape.
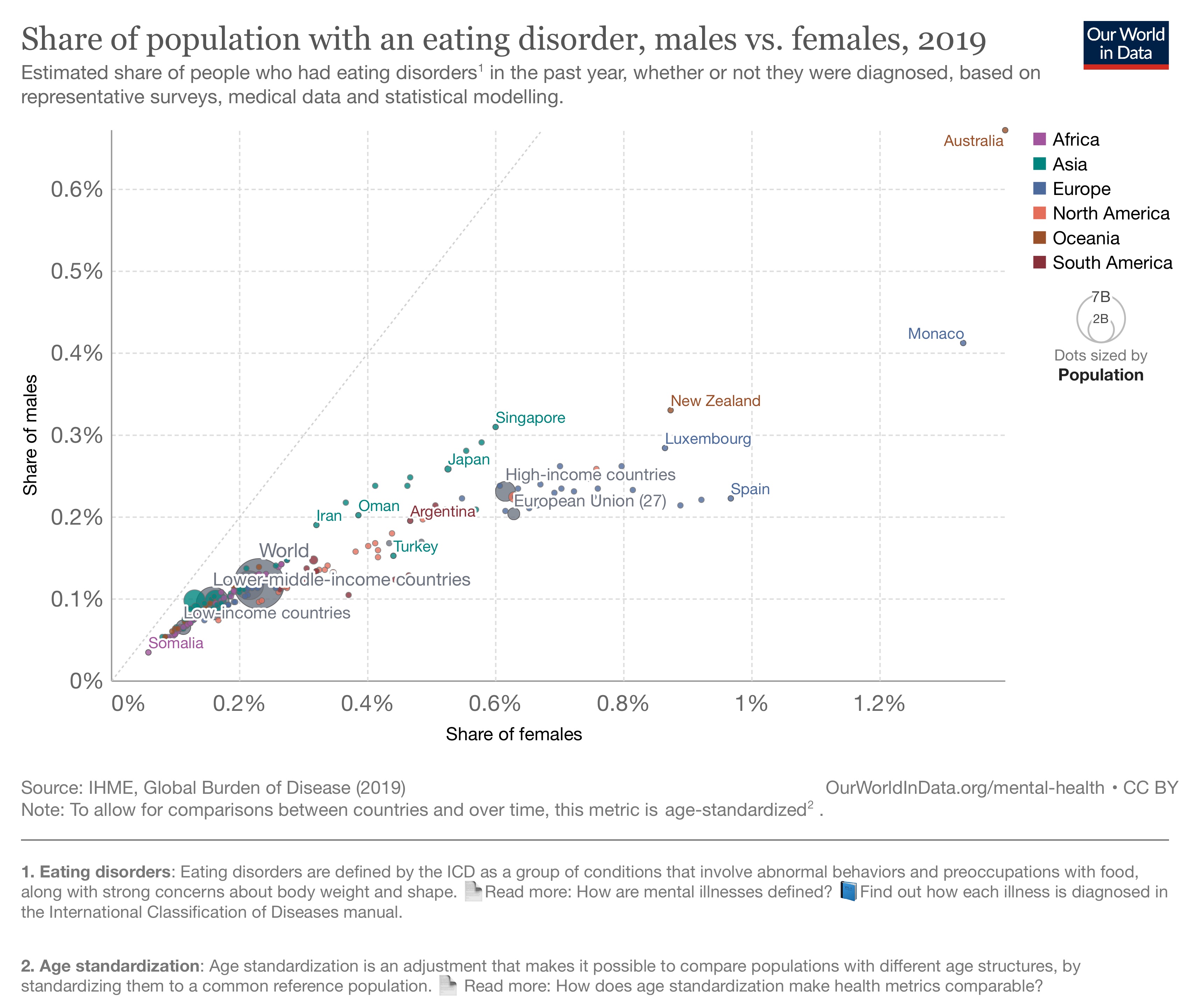
In the chart, you can see the estimated share of people who would meet the criteria for eating disorders, in men and women. Eating disorders are estimated to be more common among women (0.06–1.5%) than men (0.03–0.75%).
Anorexia
To be diagnosed with anorexia nervosa, the ICD manual explains that the patient must have significantly low body weight for their height, age, developmental stage, or weight history. Or, they must have had rapid weight loss along with other requirements. For children and adolescents, their symptoms may be the failure to gain weight as expected with age, rather than weight loss.
Their low body weight should not be better accounted for by another medical condition or a lack of available food.
They have persistent patterns of behavior aimed at reaching or maintaining an abnormally low body weight, and typically have an extreme fear of weight gain.
These behaviors can include strongly reducing energy intake (such as fasting, choosing low-calorie food, eating excessively slowly, hiding or spitting out food), purging behaviors (such as self-induced vomiting and the use of laxatives, diuretics, enemas, or not using insulin among individuals with diabetes), or increasing activity (such as excessive exercise, hyperactivity, deliberate exposure to cold, or the use of medication that increases activity).
Patients also have an excessive preoccupation with their body weight or shape, which feel central to their perception of themselves.
Bulimia
To be diagnosed with bulimia nervosa, the ICD manual explains that the patient must have frequent, recurrent episodes of binge eating. Binge eating is defined as a period when the person has a loss of control over their eating behavior and eats much more or differently than usual.
Along with this, they have repeated inappropriate behaviors to prevent weight gain, such as self-induced vomiting, fasting, the use of diuretics, laxatives, or enemas, or not using insulin among individuals with diabetes, or strenuous exercise.
They have an excessive preoccupation with body weight or shape and have significant distress about their behavior, or it significantly affects their personal life, family, social, education, work, or other areas.
To be diagnosed, their symptoms should not meet the diagnostic requirements for anorexia.
Stress disorders
These conditions are related to stressful or traumatic events or a series of events or harmful experiences.8
Post-traumatic stress disorder (PTSD)
To be diagnosed with PTSD, the ICD manual explains that the patient must have been exposed to an event or situation that was extremely threatening or horrific.9
Following the traumatic event or situation, they must have developed a syndrome lasting at least several weeks that includes all three core elements:
- Re-experiencing the traumatic event psychologically. This is typically accompanied by having strong or overwhelming emotions and strong physical sensations. Reflecting or ruminating on the event and remembering the feelings they experienced at the time are insufficient to meet this requirement.
- Deliberately avoiding reminders of the traumatic event. This can include avoiding thoughts and memories of the event, avoiding people, conversations, activities, or situations that remind them of the event. In extreme cases, they may change their environment (such as moving to a different city or changing jobs) to avoid reminders.
- Persistently perceiving the threat as being heightened. For example, being hypervigilant or excessively startled by stimuli such as unexpected noises. They constantly guard themselves against danger and feel that they, or others close to them, are under immediate threat. They might develop new behaviors that aim to ensure their safety.
To be diagnosed, their syndrome must significantly affect their personal life, family, social, education, work, or other areas.
Personality disorders
Personality disorders were previously defined as a group of different disorders that were all related to people’s behavior, perception, and social functioning. But now, they are all classified together by the ICD manual.
To be diagnosed with personality disorders, the patient must have persistent problems about themselves (their identity, self-worth, the accuracy of their self-perception, or self-goals) or their relationships (such as maintaining close and satisfying relationships, understanding other people’s perspectives, and managing conflict in relationships). These problems are visible in patterns of thoughts, emotions, and behaviors that are rigid or poorly regulated.
These problems must have persisted over a long time – at least two years – and affect a range of personal and social situations, not specific ones.
Personality disorders can be categorized as mild, moderate, and severe. But to be diagnosed, the disorder must significantly affect the person’s personal life, family, social, education, work, or other areas.
They should not be better accounted for by another mental disorder and should not be the result of another medical condition or the use of substances or medication. They should also not be diagnosed if the patterns are typical during that period of development (such as problems establishing a self-identity during adolescence) or if they can be explained by social or cultural factors.
Conclusion
Our understanding of mental illnesses continues to develop over time. They are a range of conditions that significantly affect people’s lives and are reflected in their behavior, thoughts, or relationships with others.
To be diagnosed with a mental illness, people need to meet various symptom requirements. Healthcare professionals need to exclude other conditions that can cause the symptoms and the use of substances or medications.
Republished under a Creative Commons BY license from Our World In Data. Read the original article.