Ultra-bandage: How bioelectric technology could quickly heal severe wounds
- When your skin is cut, an electric field is created which attracts cells toward the wound.
- Broken bone also emits a strong wound current.
- Supplementing the “electrome” — the combined electrical properties of our cells — may lead to accelerated healing.
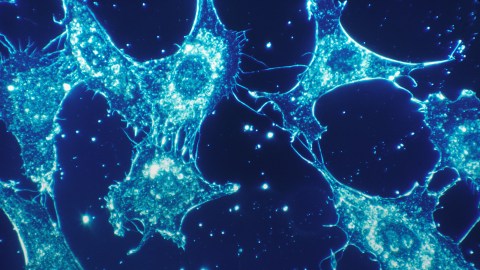
Your skin is a tightly coordinated collective of billions of cells. It’s organized into three layers of tissue called epithelium, the outside-facing of which is called the epidermis. If you’ll permit an oversimplified metaphor, you can think of your skin as a scaled-up cell membrane, but for your whole body. That’s especially true from an electrical perspective. Epithelium generates a voltage across itself. You could interpret it as an ‘all systems nominal’ signal. When your skin is intact, it generates an electric potential so that the outer skin surface is always negative with respect to the inner skin layers.
Where it gets really interesting, though, is what happens when you cut that skin. You sever the epithelial layers of the epidermis, and when that happens, all those sodium and potassium ions, which had been traveling nicely through the neat pathways offered by their gap junctions, leak haphazardly all over the place. If this were a wire you had cut, you’d be short-circuiting it, meaning electricity would flow in every direction. The neat avenues for the current are gone or smashed-up, and so the ions just pour out into every available space.
All that leaking current creates a field whose influence can be felt across some distance within the body. This acts like a combination burglar alarm, compass, and bat signal for surrounding cells. Artificially generated electric fields can drag individual cells around a petri dish. The naturally occurring field created by the wound current convinces a whole crew of them to migrate to the wound. It guides in and directs the body’s emergency workers: the keratinocytes and fibroblasts that rebuild the structure, and the clean-up crew (the macrophages). They all work together to reseal the epidermis. The electric field directs the cells to the centre of the wound. That’s your natural cathode — the big red bulls-eye towards which all the migrating helper cells in the body are marshaled.
The idea of accelerated wound healing seems to be reaching a critical mass.
This starts the repair process. And as the repairs get underway, the wound current and its associated electric field begin to fade out. By the time the wound is healed over, there is no more wound current to detect. This is how it works in all epithelial cells.
Bone is a piezoelectric material, which means it’s a tissue that can take one form of energy (the compression of running, say) and convert it to another. For example, the stress of your footfalls on your bones makes them grow stronger because the charges bone cells generate in response to this mechanical activity get translated into electric signals that promote bone growth. Bone also emits strong wound currents when it breaks.
In short, you can’t talk about a living system without recognizing its electrical component. We are nothing without electricity. So if the body naturally uses its own electricity to heal wounds, what if we could learn how to control it?
Faster healing
Researchers in Scotland found that if they used channel-blocking drugs to inhibit sodium ions, thereby interrupting the electrical signals sent by the wound current in rats, their wounds took longer to heal.
But was the opposite true? Could we also speed up the healing process by amplifying our body’s natural electricity? A spate of clinical trials over the past decade increasingly suggests that the answer is yes. Perhaps the most harrowing kinds of wounds are severe bed sores, which can take months to years to heal (if they heal at all) and attack tissue, muscle, and bone deep beneath the skin. Most of the research using electrical stimulation to heal wounds in humans has been done in these kinds of wounds — like deep brain stimulation, this is a method of last resort when nothing else seems to help. After many years of these kinds of experiments, two groups of scientists conducted meta-analyses and concluded that amplifying the natural wound current with electrical stimulation almost doubles their healing rate.
Nor was the effect limited to skin; since the 1980s, a growing body of evidence hinted that the same kind of small electrical currents could accelerate healing in bone fractures, and some suggested it might even help treat osteoporosis. It helps new blood vessels grow into wounds faster and is also beginning to be seriously examined for eyes. Electrical stimulation has even been shown to be effective at aiding skin transplants — it seems to help the new skin take.
There’s a catch: the results of all these types of experiments have been broadly positive — but also inconsistent and unpredictable. Because we don’t understand the precise mechanism by which the electricity is speeding the healing of the wound, we can’t do anything targeted to enhance or improve — or even standardize — the stimulation. And that makes things hard for any doctors hoping to use electrical stimulation on their patients.
The physiologist Min Zhao was able to vastly advance this understanding in 2006, when he and the geneticist Josef Penninger undertook the first-ever controlled experiment aimed at pinning down some of the genes that get switched on by electric fields on wounds. This work was reported widely in the news — it finally brought electricity into the legible zone of genes. This was some of the earliest, most robust and tantalizing evidence for the epigenetic power of the electrome.
The Dermacorder
The next thing to do was find a way to measure the actual electrical field of human wounds. Existing electrotherapy devices apply current with no insight as to what effect it has on a person’s own bioelectricity. To change that, you need a device that can help identify whether a person has an abnormal or malfunctioning wound current. No tool had ever been capable of measuring the electric field in the air next to dry mammalian skin — it had always been done on wet frog skin in the controlled conditions of a lab. In 2011, Richard Nuccitelli created a non-invasive device that could deal with human skin, allowing our injury currents to be closely observed. The Dermacorder could sense whatever the nearest voltage is. Hold it up to the skin and it maps the voltage on its surface and correlates it with the depth of the wound. That gives you a topographical, three-dimensional electrical map of the wound. This was the first tool a physician could actually hold and use on a person.
It vastly deepened the understanding of how electricity works in wound healing. Nuccitelli found a strong correlation between the magnitude of the wound’s electric field and the progression of the healing — it peaks at injury, slowly decreases as the wound heals, and returns to undetectable when healing is complete. More interesting, though, was the relationship between the strength of a person’s wound current and their ability to heal. People with weak injury current healed more slowly than those whose injury current was ‘louder.’ Most interesting of all: wound current strength wanes with age, emitting a signal that is only half as strong in people over the age of 65 as it is in those under 25.
With better measurements came better experimental results. In 2015, Nuccitelli and Christine Pullar applied electrical stimulation to wounds and, mapping it with the Dermacorder, were able to coax new blood vessels to form, accelerating the healing in all their patients.
The idea of accelerated wound healing seems to be reaching a critical mass. In 2020, DARPA gave a team of researchers including Zhao $16 million to develop a next-generation wound-healing system. This will not be a sticking plaster like the kind you use when you nick yourself chopping vegetables. The bandage is intended to heal major traumatic wounds, so it will recruit bioelectric healing of multiple kinds of tissues at once — and speed up healing in all of them.