Ask Ethan: What is a woman?

- For most of human history, we’ve by default sorted people by sex, gender, and sexual preference into binary categories: where there are only two options to choose from.
- In most situations, however, the binary extremes only capture the majority of the population, further excluding and marginalizing a population of people that are already in the minority.
- By capitalizing on our modern, expert understanding of science and medicine, we can come to draw informed conclusions for what actions we ought to take to best serve — and protect — all members of our society.
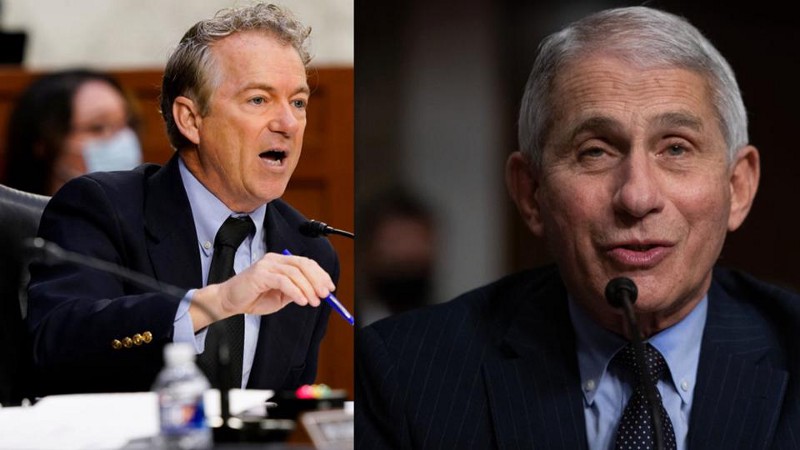
I know, I know. “Ethan, you’re an astrophysicist. What in the world are you doing writing about this topic?” Every week, I get questions submitted to me on a variety of media platforms from all over the world, and I do my best to fairly consider each one, and then to provide the absolute best answer I can according to our modern scientific understanding of reality. I’ve seen many, many people that I know, very recently, espouse very strongly held beliefs on the topics of:
- sex,
- gender,
- mental health/illness,
- and transgender issues,
among others. But while people are quick to make recommendations for what behaviors and procedures should be normalized and which ones should be marginalized or even outlawed, very few of those same people can scrupulously point to the science behind those issues, and that’s where I can help: by taking off my astrophysicist hat and putting on my science journalist hat. With that said, this week’s inquiry comes from Tom Ruen, who suggests this topic:
“Hi Ethan. I believe you are the most productive scientific communicator in America, and I don’t know how you do it. But if you want to understand the trans-backlash… understand faith-based science is not science. […] I know, life is busy, but there are smart people who have looked deep, without having anything to lose personally, so they speak up now, and we have no excuse to ignore their conclusions because they are harsh.”
So I went to a number of experts in biology and medicine, and — while keeping them all anonymous (except for links to sources) — here’s what I can put together as far as “what is true” about sex, gender, and medical care for trans and intersex individuals. I think everyone, regardless of your political stance, would benefit from learning these scientifically true facts.
One simple-seeming question that you might think to ask is, “What is the sex and gender of a human being?” But if you try to go about answering it in a simple, unambiguous way, you’d find that no matter which method you tried to use to categorize people, none of them successfully apply to 100% of the population.
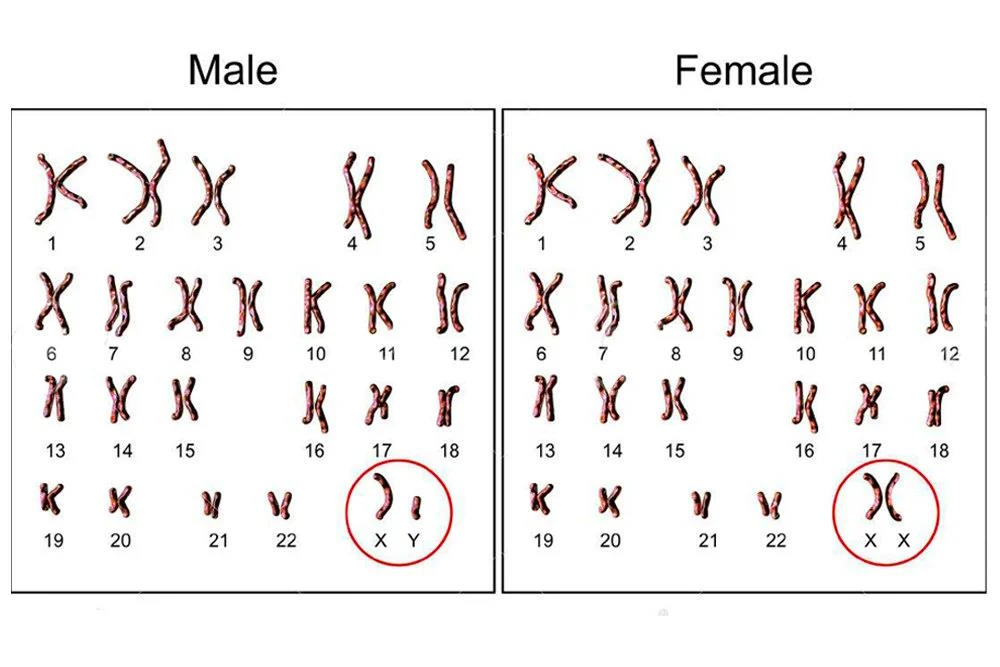
- You might, with a little biological knowledge, try to sort people by their chromosomes: if your chromosomal makeup has “XX” within it, you’re female; if you have “XY” within it, you’re male.
- You might, either instead or additionally, try to sort people by their reproductive organs: if you have a penis, scrotum, and testicles, you’re male; if you have a vagina, clitoris, and uterus, you’re female.
- You might choose, alternatively, to look at the reproductive gonads a person possesses: if you have ovaries, you’re female; if you have testes, you’re male.
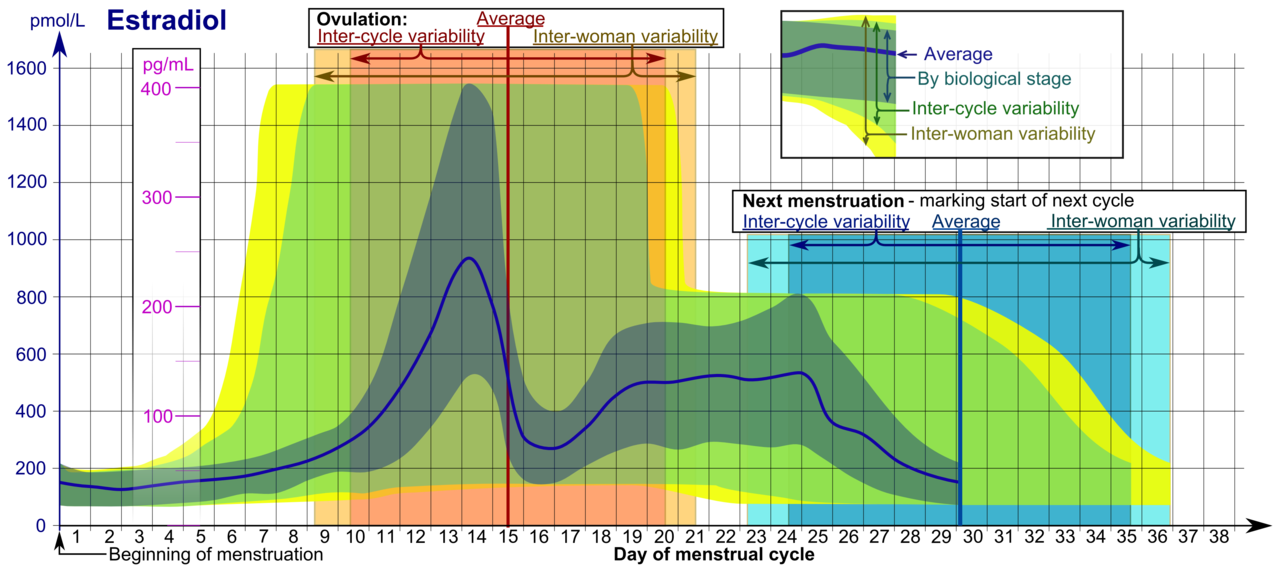
- You might look at the sex hormone levels present within their bodies: the mixes of estrogens (including estradiol), androgens (including testosterone), and gestagens (like progesterone) that the individual possesses, with clear differences between the typical levels found in male and female bodies.
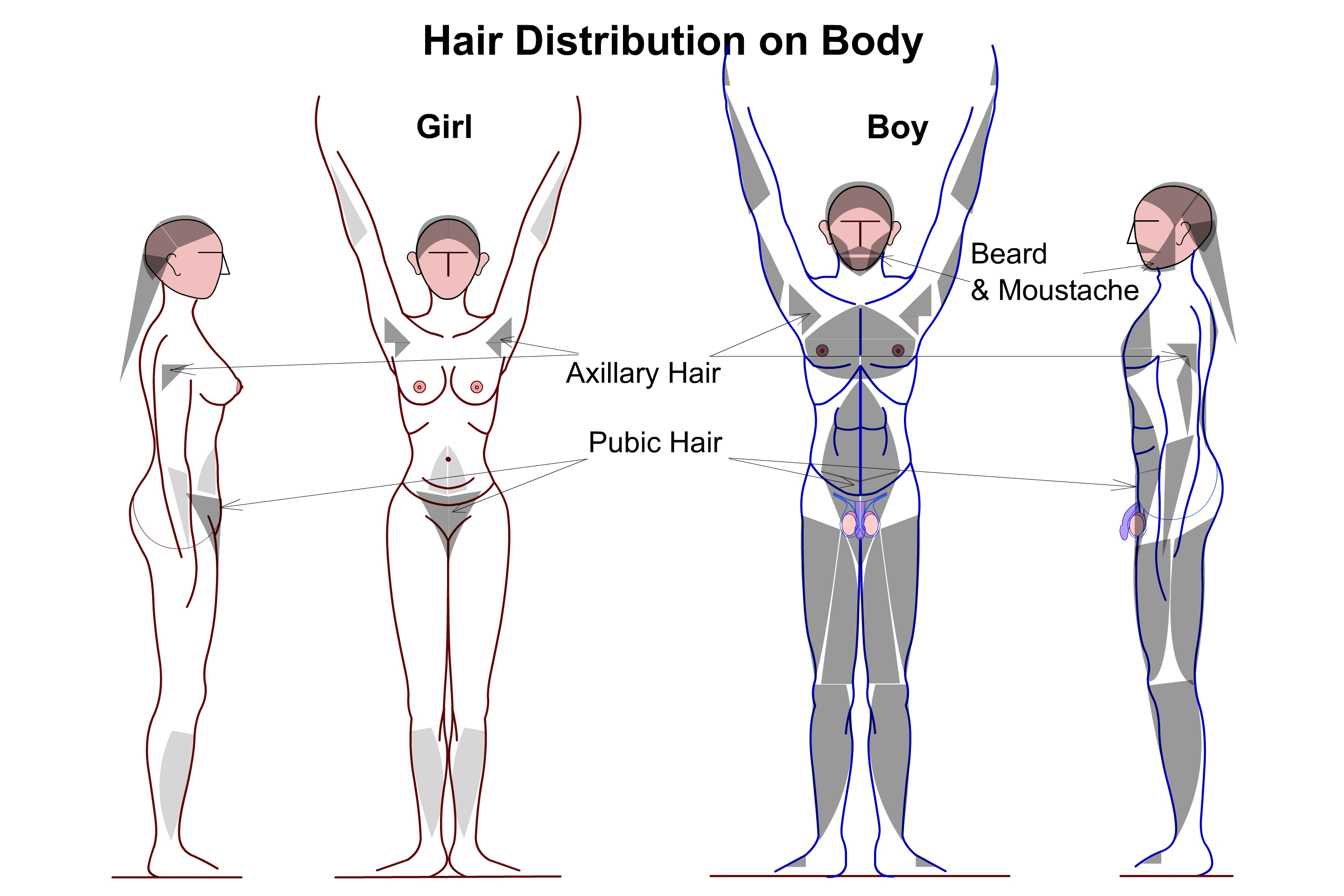
- Or you might look for other characteristics that are commonly used to distinguish between male and female human bodies: things like
- breast size and the ability to lactate,
- the size and proportions of the chest, waist, and hips,
- height,
- the amount of body and facial hair,
- the relative amounts of muscle mass and body fat,
- vocal pitch and lung capacity,
- or the size of the heart in full-grown adults.
Every animal has traits such as these, and from a biological perspective, they’re classified into three basic categories.
The first category — your sex chromosomes — determines what we typically call your biological sex. “XX” is the genotype, or underlying genetic code, for female humans; “XY” is the genotype for male humans.
The second category — which includes internal and external reproductive organs, reproductive gonads, and sex hormone levels — are known as primary sex characteristics. In contrast to the genotype, which refers to the underlying genetic code in their DNA, these are phenotype characteristics: directly observable in living organisms. Humans are born with these characteristics and, when they reach sexual maturity, gain the ability to ejaculate semen if male or menstruate and give birth if female.
And the third category — which includes the long list, above, of physical differences that are relatively easy to observe — are known as secondary sex characteristics. They don’t have anything to do with a person’s reproductive capabilities, but are rather examples of differences, on average, observed between individuals in any sexually dimorphic species. Male lions have manes; male peacocks have long, brightly colored tail feathers; male deep-sea anglerfish are diminutive and must latch onto and fuse with female fish to obtain nutrients.
From a scientific perspective, most human organisms can be fairly easily categorized into male or female members, but in many cases, it isn’t so clear.

You might be puzzled if this is the first time you’re hearing about this, and you might be tempted to dismiss those who don’t neatly fit into a “clearly male” or “clearly female” description across all three categories as outliers, anomalies, or even as abnormal, but that would be a mistaken approach. In science, we study what exists in nature, what the natural properties of the things that exist are, and try to understand the mechanisms behind their developmental pathways that led to them becoming the way they are.
For instance, there are many examples of people whose chromosomal makeup is “XX” but most of their primary and secondary sexual characteristics are male. This condition, although rare (occurring in about 1-in-20,000 male newborns) is known as de la Chapelle syndrome, and most often arises because the gene sequence for a DNA-binding protein that triggers the formation of testes and other male developmental features has gotten encoded into the X-chromosome coming from the genetic father, although it can arise (in 10-20% of cases) for other, sometimes unknown reasons. XX males can have extremely variable presentations for their sex characteristics; some develop as males and never know that they have “XX” for their chromosomal makeup, while others possess more ambiguous sex characteristics and benefit from hormone therapy and/or surgery, with most affected individuals benefiting from being treated with testosterone at the onset of puberty.

There are also numerous examples of people whose chromosomal makeup is “XY” but their primary and secondary sexual characteristics express as female, including a similarly-rare condition (about 1-in-80,000) known as Swyer syndrome. People with Swyer syndrome typically have female reproductive structures both internally and externally: a vagina, labia, clitoris, and usually a uterus and fallopian tubes. However, they only have non-functional gonads: small and underdeveloped structures called streak gonads. (When Swyer syndrome is discovered, these streak gonads are normally removed, as they’re at high risk for developing cancer.)
Hormone replacement therapy is often useful to individuals with Swyer syndrome, which helps their breasts and uterus to grow; with HRT, women with Swyer syndrome usually menstruate as well. In addition, although they do not produce eggs, they can become pregnant with either donated eggs or implanted embryos. There are a variety of genetic markers for it, but not every case can be linked to an identifiable cause.
Although there are several factors that determine whether a person will develop with traditionally male or female primary and secondary sexual characteristics, the presence or lack of specific hormones and proteins in the embryonic stage — as opposed to their underlying “XX” or “XY” genotype — seems to be the primary factor.

Additionally, there are several other sex genotypes that are present in the human population beyond the two most common options of XX and XY. The most common ones (although there are others) include:
- XXY, which leads to Klinefelter syndrome in males, with primary features like large height, weak muscles, infertility, and several poorly developed male sexual characteristics. This affects approximately 1-2 in 1,000 live male births.
- XYY, which typically leads to normal male development in most ways, but can lead to larger height, heads, and teeth, increased risk of learning and speech disabilities, and increased risk of several mental health disorders. This affects about 1 in 1,000 live births.
- X0, which leads to Turner syndrome in females, and is caused by a partially or completely missing X chromosome. It has a number of physical and psychological signs, including short height, heart defects, neck webbing, infertility, and delayed or completely absent puberty. It is typically treatable with various hormones, like HGH and estrogen, and affects about 1 in 2,000 female births.
These three cases — of XXY, XYY, and X0 — are classified as “intersex” disorders, in the sense that they are disorders of sex development in humans. This type of intersex disorder typically doesn’t result in a discrepancy between internal and external genitalia, but those who have it do exhibit problems with sex hormone levels, overall sexual development, and (obviously) having altered numbers of sex chromosomes.

However, there are three other major categories of intersex disorders that do include a discrepancy between internal and external genitalia, including one class we haven’t yet mentioned: true gonadal intersex individuals, where both ovarian and testicular tissue are present within their bodies. Most such individuals can potentially give live birth (a traditionally female trait), but at least one individual has been documented as fathering a child. It may yet be possible for some people who fall into this category to self-fertilize, a phenomenon never before seen in humans but that’s widespread throughout the animal kingdom.
All told, humans follow what’s known as a bimodal distribution when it comes to sex and gender. Most individuals fall into one of two primary categories:
- Their chromosomes are male (XY), their primary sex characteristics are all male, and their secondary sex characteristics are all (or mostly) male.
- Or, their chromosomes are female (XX), their primary sex characteristics are all female, and their secondary sex characteristics are all (or mostly) female.
However, it’s bimodal, meaning most people fall into one of these two categories, but some people exhibit traits that place them in the overlapping middle between the two, not binary, which would mean these were the only two options. Medical experts report that between 0.05% and 0.08% of all live births exhibit evidence of ambiguous genitalia, and that far greater numbers of people have a subtler form of intersex condition that only appears later in life, with the most common arising from congenital adrenal hyperplasia, or CAH. Although what’s called “classical CAH” is the best studied form of this condition, it’s actually non-classical CAH that’s far more common: affecting somewhere between 0.5% and 1% of the general population. (Although a notable 2015 review put the estimate higher: at 1.7%.)

Think about even that conservative figure of 0.5%. That’s 1-in-200, meaning that over 1.5 million Americans and more than 40 million people worldwide, at least, exhibit some type of intersex condition, and possess inherent biological traits that are neither 100% male nor 100% female. For most of human history, such individuals were considered monsters and were often treated as such. During the 20th and even into the 21st centuries, most physicians would surgically assign a gender to a newborn identified as intersex, with many noting that,
“The reconstruction of female genitalia was more readily performed than the reconstruction of male genitalia, so ambiguous individuals often were made to be female.”
Is this a monstrous thing to do? The difficult answer is: sometimes. You must understand that we all have, internal and inherent to us, a sense of what we call our gender identity. For most of us — especially for most typical males and most typical females — our gender identity matches, aligns, and is congruent with our assigned gender. This sense of gender identity develops in stages, where:
- Around age 2: children recognize physical differences between boys/girls and men/women.
- By age 3: children label themselves as either a boy or a girl.
- By age 4: children have a (most commonly) stable sense of their gender identities.

If you’re a human whose gender identity matches your assigned gender, congratulations! You’re like most people, and you’re unlikely to suffer from a deep sense of unease and dissatisfaction with the assigned gender of your body: a condition known as gender dysphoria. However, just as a small percentage but a significant population of humans fall outside of a binary description of gender, a small but significant percentage — a percentage that still has large uncertainties associated with its estimates but is likely to be close to the percentage of people who fall outside of the gender binary — do experience gender dysphoria.
Very recently, a doctor who had written, in 2001, that “feminizing genitoplasty on an infant who might eventually identify herself as a boy would be catastrophic” did indeed perform a surgery on a 16-month-old intersex baby, assigning them a female gender. The child would later go on to develop a male gender identity, resulting in precisely the catastrophic situation that one would hope to avoid: a case of gender dysphoria that was created by early, unnecessary medical intervention.
But, used properly, the same healthcare tools and technologies that have been used to treat intersex people, notably hormone therapies and surgical options, can be very successfully used to help those with gender dysphoria achieve an assigned gender that’s far more in line with their gender identity, irrespective of their assigned gender at birth.
There are additional reasons to appreciate the diversity in sex hormones and sex chromosomes as well, as ignoring them can have severe health consequences. A novel cancer therapy was administered equally to both men and women, and researchers quickly found that women were dying at twice the rate of men. Estrogen influences the response of cells to strategies used when fighting HIV, and males and females of different ages have different immune responses in patients with COVID-19. If we want the best medical care for everyone — cisgender, transgender, and those yet to decide — the biological mechanisms contributing to these differences must be investigated and understood.
Although there has been a lot of concern trolling about individuals, particularly children, who undergo this type of gender reassignment surgery, there are a few high-quality studies that look at the regret and recidivism rate for these surgeries: those who either regret having the surgery at all or who de-transition from their gender reassignment surgery. The results of these studies revealed:
- That only 16 out of 3398 (0.47%) of patients in a UK study experienced transition-related regret.
- That up to 8% out of 28000 trans people in the USA experienced some sort of detransition, but that a solid majority of those detransitions were temporary and driven by societal, financial, and/or familial pressures.
- That a 50-year study of 767 people who applied for gender reassignment surgery in Sweden found that around 2% experienced some sort of transition-related regret, but that percentage has declined over time, and declined sharply after the year 2000.
- And that 97% of people who transition are happy with their decision to transition. Of those who detransition, the overwhelming majority cite familial and societal pressures for doing so, with only a small fraction citing internal identity reasons.
These detransition and regret statistics are comparable to the percentage of women (2%) who regret breast augmentation surgery, and smaller than the percentage of men (6%) who regret their decision to get a vasectomy. In other words, if you’re asking the question, “Have individuals with gender dysphoria been transitioning at rates that indicate we are overmedicalizing them, or medicalizing them too early for them to have a good sense of their actual gender identity?” the answer seems to be that there is no data supporting those assertions at present.

However, it’s absolutely true, and very well-documented, that trans and non-binary individuals are far more likely to experience violence, mistreatment, harassment, and sexual assault because they were transgender. This includes in school, from family, and in the workforce; the rates of all of these are higher than for any other documented group. Furthermore, the incidence of suicidal ideation (over 80%) and of making suicide attempts (40%, at least) are extremely high for this group: the highest of all documented marginalized groups. The top factors contributing to these rates are lack of family support and rejection, particularly from the individual’s parents.
To me, that’s the most important statistic: that the suicide attempt rate for trans youth, which is estimated to be 43-45% if they’re not well-supported in their gender identity by at least one parent, drops by more than a factor of 10, to around 4%, if they do have strong parental support in their identity.
I can’t, in good conscience, make health or medical decisions for anyone else — for adults, for youth, or for parents of those with gender dysphoria — as that’s a set of decisions that must be made between individuals and families and their doctors. But I can unequivocally state that intersex, trans, and non-binary individuals — including children, adolescents and adults — are not monsters in any way; they’re simply a normal minority that’s a healthy part of any human population. We all have more to learn about sex and gender, but the takeaway lesson for any parent is that failing to love and support your child, irrespective of which medical interventions are and are not taken at any particular age, is the most detrimental thing you can do to them.
For more information and another perspective on gender, please enjoy this Big Think video by gender theory professor Dr. Judith Butler.
Send in your Ask Ethan questions to startswithabang at gmail dot com!