This Is How ‘False Positives’ And ‘False Negatives’ Can Bias COVID-19 Testing

If we’re going to open major workplaces, we have to be ready for this enormous information gap.
When it comes to knowing your medical status, the ideal scenario is to have a 100% accurate, widely available, easy to administer and evaluate test. But a variety of factors that can be specific to whatever test you’re performing can lead to a less accurate test, where either false positives or false negatives result. Even if a test is extremely accurate, a small false positive or false negative rate can lead to disastrous consequences on both an individual and societal level.
In the case of the novel SARS-CoV-2 virus and the COVID-19 illness that it causes in humans, the goal of testing is very simple: to identify who is infected and to isolate them, thereby preventing the infection of others. But without a perfect test, false positives and false negatives can lead to significantly worse outcomes. Here’s what we all need to be aware of.

If we could approach the world from an all-knowing point of view, we would be able to know, with no errors, who has a positive status and who has a negative status for whatever condition or affliction we’re looking at. The ideal diagnostic test would give everyone who was positive a positive result, and everyone who was negative a negative result. That’s what medical testing always aspires to.
But in real life, we have both false positives and false negatives. This is what they mean.
- False positive: the person you’re testing is actually negative, where they don’t have the condition you’re testing for. But the test returns a positive result anyway. The rate of false positives is the number of false positive results divided by the total number of true negative results.
- False negative: the person you’re testing is actually positive, afflicted with the condition you’re testing for. But the test, when administered, gives a negative result. The rate of false negatives is the number of false negative results divided by the total number of true positives.
Depending on what you’re testing for and what these rates actually are, the consequences of either one could be devastating. If you’re testing for a rare but lethal disease, a high false positive rate is a nightmare. For example, let’s assume you have a disease where the test has a false positive rate of 1% (and no false negatives), but only 1-in-10,000 people actually have the disease.
If you perform the test on 1 million people, you’ll wind up with a total of 10,099 positive test results out of your total sample of 1 million. But of those positive results, only 100 people will actually have the infection. You’d needlessly scare — and, if it was part of the treatment, isolate and quarantine — 9,999 people if you relied on those test results. (In other words, a total of 99% of the positives would be false.) The ELISA test for HIV, which has a greater-than-1% false positive rate, has been criticized for exactly this reason.
On the other hand, false negatives can be particularly dangerous in a very different way: by giving the “OK” those who test negative (but who are actually positive) to engage in potentially risky behaviors. Large false negative rates can lead to very troubles outcomes when the affliction is either highly contagious or where very large numbers of people are expected to be positive.
A classic example is a home pregnancy test. If you test positive, you’re pregnant; if you test negative, you’re not. An estimated 20 million Americans take a home pregnancy test annually. Although these tests are touted as being 99% accurate, some evidence indicates that false negatives can occur in up to 5% of those taking the test. With an estimated 6.2 million pregnancies per year in the USA, a 5% false negative rate could lead to 310,000 pregnant women annually consuming alcoholic beverages, exposing their unborn child to a myriad of risks.
10%) false negative rate. (Robin Utrecht/SOPA Images/LightRocket via Getty Images)” enhanced=”” style=”box-sizing: border-box; position: relative; display: block; margin-top: 0px;”>

In reality, most tests can have both false positives and false negatives associated with them. (Even home pregnancy tests can have false positives.) For the widespread tests we’ve been using for SARS-CoV-2, which causes COVID-19 in humans, both false positives and false negatives are ubiquitous, but can have vastly different consequences.
Someone who tests positive, whether that’s true or false, will need to be isolated and monitored, and everyone who has come into contact with them will also need to be tested and treated as though they’re possibly infected. In order to cease infecting others, sheltering in place — preferably separated from the other members of their household — is the proper course of action.
But someone who tests negative, whether it’s a true or false negative, will be allowed to participate in society at whatever level is deemed acceptable.

And this is a big deal: recent data suggests that approximately 15% of all tests conducted in the United States are returning false negatives, meaning that of every 100 individuals infected with COVID-19, 15 of them are told they don’t have it. If we were to have 1 million infected individuals in the country, and every one of them got tested, 150,000 possibly contagious individuals would test negative and be given the “all-clear” to neither quarantine nor self-isolate.
Even if testing were perfect — if everyone in the country were tested on even a biweekly or weekly basis — a test with such high levels of false negatives would be unacceptable. Although there are many epidemiological reasons why this is true, it’s easy to illustrate with one simple example: the idea of a superspreader event.

An enormous fraction of the COVID-19 cases in the United States are clustered together, meaning that the virus tears through the same facility, workplace, or isolated area all at once, infecting a significant fraction of the population there. Even one infected individual can lead to hundreds or even thousands of others being infected at a single location. Of the top 30 largest clusters identified thus far, 29 of them are nursing homes, prisons, and meat-packing plants. (The lone exception is the US Navy Battleship Theodore Roosevelt.)
If even one person who is infected were to report to such an environment, everyone who passes through that facility is now potentially at risk. Even if workplaces were to require a negative test from all employees before allowing them to return to work, the high rate of false negatives ensures that many of those workers are likely to carry COVID-19. Even one infected individual can potentially infect an entire workplace.

The latest statistics show that approximately 1 million American residents, or about 0.3% of the population, are actively infected with COVID-19 right now. (Note: this includes a positive test for COVID-19, and does not account for false positives, which also exist.) If this number — which many contend is likely an undercount — were actually representative of the entirety of the number of infected Americans who tested positive and are positive for SARS-CoV-2, then that false negative rate of 15% would translate into an additional 170,000 infected who inaccurately tested negative.
Now, imagine that you encounter one of those 170,000 people who returns to a world that’s re-opened. Maybe they’re your hairdresser. Or your server at a restaurant. Or your cashier. Or your boss. Or, simply, your customer. Each infected individual, even with all the social distancing and isolation measures we’ve implemented, is still infecting an average of 0.9 people.
With such a large number of infected individuals, including a large number that don’t know they are infected (or erroneously think they aren’t because of a negative test), the only responsible course of actions is to behave as though everyone outside of our immediate household is potentially infected, and has the potential to pass that infection onto us and others.
Even though the true infection rate is not known, it is a near certainty that no locations within the United States have achieved herd immunity. According to Anne Schuchat of the CDC’s COVID-19 Response Team:
Preliminary results from serologic surveys suggest that even in the U.S. regions with the largest numbers of recognized cases, most persons have not been infected and remain susceptible. Therefore, sustained and concerted efforts will be needed to prevent future spread of SARS-CoV-2 within the United States.

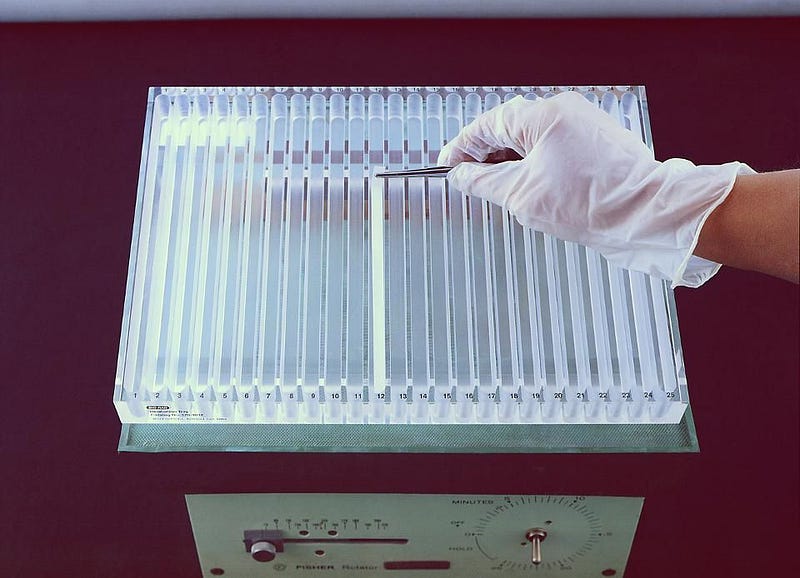
There have been many plans touted to increase testing, including batch testing, but the problem of false negatives remains. The more individuals we bundle together, the more impactful a false negative becomes, as dozens or even hundreds of individuals can be deemed negative when they are not with just a single series of tests. Most of us are still susceptible to a SARS-CoV-2 infection, and avoiding potentially transmissible contact with all infected individuals is the only way to ensure we don’t become at risk.
Both false positives and false negatives pose their own unique dangers wherever any sort of testing occurs, but false negatives are particularly dangerous for COVID-19. The large false negative rates of all ubiquitous COVID-19 tests make it likely that if you’ve been exposed and have symptoms, you might be infected after all, even if you’ve tested negative. Until we have better and more widespread testing, we simply won’t know.
Ethan Siegel is the author of Beyond the Galaxy and Treknology. You can pre-order his third book, currently in development: the Encyclopaedia Cosmologica.