How the brain’s vagus nerve tastes sugar in the gut

- Our craving for sugar originates in the gut, which is able to distinguish between nutrients and guide eating behavior by sending rapid subconscious signals to the brain.
- A study published earlier this year showed that inhibiting the activity of certain cells, or blocking glutamate receptors, in the guts of mice abolishes their preference for sugar over artificial sweetener.
- Gaining a better understanding of the role of the gut in sugar consumption could help address the obesity epidemic by pointing to new ways of promoting healthier eating habits.
Most of us find sugary foods pleasurable to eat, and we consume too much of them. Despite the introduction of artificial sweeteners, the over-consumption of sugar is a major contributor to the global obesity epidemic and metabolic disorders such as diabetes.
There is, therefore, a need to understand how we detect sugar and why so many people choose to consume so much of it.
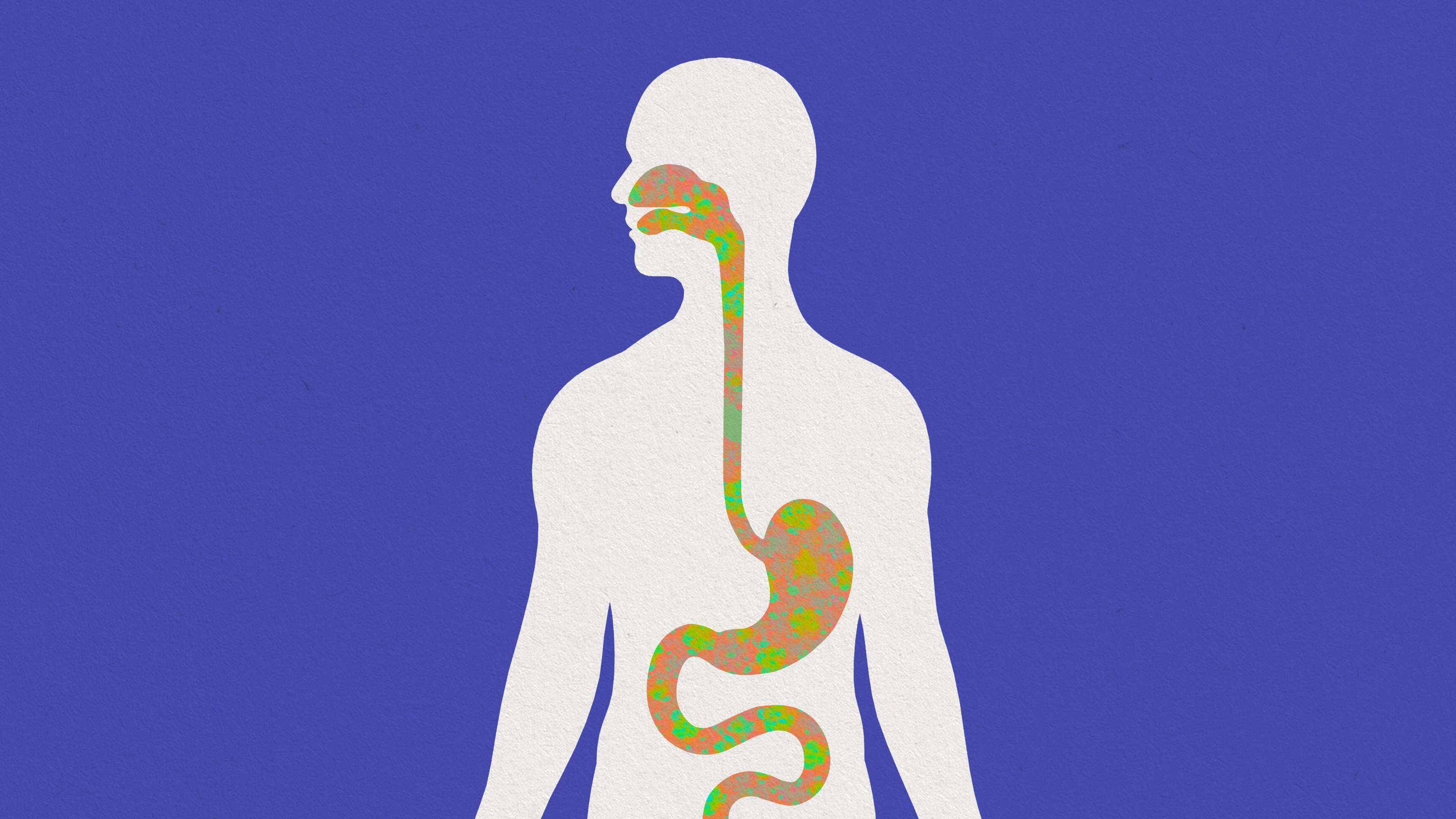
Research into how sugar affects the brain dates back at least to the 1940s, but in recent years our knowledge has accelerated. Although we detect sweetness with the taste buds in the tongue, our craving for sugar originates in the gut, which can distinguish between nutrients and guide eating behavior by sending rapid subconscious signals to the brain. We now know that these signals are sent by specialized neural cells in the gut; they can override conscious processing to make us seek out sugary foods, despite knowing they are bad for us.
In the 1940s, the physiologist Edward Adolph performed a series of experiments designed to test the relationship between food quantity and nutritional content. He fed rats a diet consisting of cellulose, which animals cannot digest, and found that they ate more but did not consume more calories.
A few years later, further experiments showed that milk injected directly into rats’ stomachs was rewarding and led to learning. In the late 1960s, the role of gut-brain signaling was confirmed in a classic study in which rats were given differently flavored sweet solutions paired with gastric injections of eggnog or water. Later, when given the choice of the solutions alone, they chose those that had previously been paired with the eggnog.
Sugar receptors
Sugar is detected by both the tongue and the gut by taste receptors, glucose transporter proteins, and ATP-gated potassium channels. These proteins are also found in the pancreas, fat cells, and brain, and all of them contribute to detecting sugar before and after it has been absorbed.
Until very recently, it was widely believed that sugar detection in the gut is mediated by hormone-secreting endocrine cells. In the past decade, however, it has emerged that sugar-detecting cells form synaptic connections with the vagus nerve — showing that the cells are in fact specialized neurons, which were dubbed “neuropod” cells.
Neuropod cells express a protein called sodium-glucose co-transporter 1 (SGLT1), and respond to glucose (the basic component of all sugars) by releasing the excitatory neurotransmitter glutamate. This activates fibers in the vagus nerve, which signals up to the brain within milliseconds.
A study published earlier this year showed that inhibiting neuropod cell activity or blocking glutamate receptors in the guts of mice abolishes their preference for sugar over artificial sweetener. This confirms that neuropod cells guide the consumption of, and preference for, sugar, but it is still unclear whether these cells are also necessary for the development or memory of this preference.
Brain circuits
In the brainstem, vagus nerve terminals form synaptic connections with fibers that project to the dopamine-producing reward circuitry in a subcortical structure called the basal ganglia, and also to the hypothalamus, which regulates eating behavior.
The brain’s reward circuitry contains two distinct pathways, which appear to perform different roles in learning about sugar consumption. The mesolimbic pathway appears to assign reward values to sugary foods, whereas the nigrostriatal pathway seems to be necessary and sufficient for the reinforcing effects of absorbing sugar.
The hypothalamus contains populations of neurons that control food intake, and whose activity is suppressed by food consumption. Experimental activation of these cells leads mice to seek and then consume food, whereas inhibiting them makes the animals lose their appetite.
Sugar detection is now thought to occur continuously via the epithelium in the mouth to the gut. But eating is a multisensory experience that begins before food even enters our mouths. Thus, the sight, smell, and even texture of sugary foods triggers the brain’s feeding circuits, which anticipate its reward value.
Inside the mouth, the food then activates taste receptors, which then signal the reward pathways, eliciting pleasure. Down in the gut, neuropod cells detect the sugar and rapidly signal the brain via the vagus nerve.
Gaining a better understanding of the role of the gut in sugar consumption could help address the obesity epidemic by pointing to new ways of promoting healthier eating habits.